The international response to the Ebola outbreak has been limited, leaving Uganda more isolated than it should be
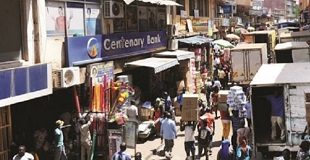
COMMENT | IRENE ATUHAIRWE DUHANGA | With news of Uganda announcing a three-week lockdown in two districts and the first Ebola death in Kampala — the capital city of over 3 million living in close proximity — it’s time the world wakes up to the threat of this latest outbreak.
The international response thus far has been muted. The U.S. government announced enhanced screening for passengers who have been in Uganda, yet the global community must recognise the most effective way of stopping this outbreak is by focusing our efforts on the front line itself.
While it may be a government’s right to take proportionate public measures to protect its citizens, splashy announcements of enhanced screening and potential travel bans are not the right answer to containing this virus and stopping its spread beyond the borders of Uganda. The best place to stop an outbreak is at its source.
“In the long term, this latest outbreak underlines the critical need to invest in health system resilience — built on the strong foundations of much greater investment in the health workforce.”
The new screening measures mark an escalation in the international response since the outbreak was declared on Sept. 20. It is the first time since the COVID-19 pandemic that such emergency measures have been taken to limit the spread of a virus.
But this overt signal falls short. We also have a moral obligation to scale up wise and thoughtful measures to protect those directly in the firing line. Not only will this save lives; it will also reduce the risk of the virus spreading; a new, more infectious strain of Ebola from emerging or — as too often disregarded — losing more health care workers to attrition or death from another infectious outbreak.
In Uganda, the Ebola outbreak, coming hot on the heels of the COVID-19 pandemic, finds a vulnerable health system barely recovering from health worker burnout, stigma, mistrust, and depletion of essential resources. Punitive responses from the international community only aggravate the vulnerability and fuel stigma.
That’s why our organisation is working hand in hand with the Ugandan government on the ground to fight the outbreak. We’re supporting rapid response teams to contact trace in the outbreak epicenter, helping to disseminate information and communications materials at the local level — and strengthening health worker capacity and resilience in high-risk cities and locations including at Mulago National Referral Hospital in Kampala.
We’re supporting training of health workers at facilities across the country on Ebola infection prevention, isolation, and personal protective equipment protocols and strengthening emergency preparedness in 25 hospitals.
Yet despite the very recent experience of the pandemic, the international response to the Ebola outbreak has been limited, leaving Uganda more isolated than it should be in the struggle to address this new threat. We, and our partners, urgently need the global community to step up with funding for more than just surveillance — to provide, train, and support well-equipped and well-protected health workers to confront this outbreak head on.
The Ugandan government has acted rapidly, leveraging experience from previous outbreaks to institute measures including field testing, contact tracing, and isolation. This outbreak, however, still has a high risk of escalating. The last outbreak of this strain of the Ebola virus in Uganda claimed 224 lives, including potentially more than 40 health workers in 4 months according to government figures.
As of Oct. 16, there have been 60 confirmed cases and 24 confirmed deaths in 26 days according to the country’s ministry of health — a relatively steep epidemic curve mainly in rural areas with a relatively sparse population. Seeding to urban, populous cities will complicate surveillance and increase the attack rate.
Spread through bodily fluids rather than air, Ebola is a different virus to COVID-19. However, this does not make it any less dangerous. With death rates that have historically reached up to 90% and no vaccine or approved treatment for this particular strain, it has the potential to cause serious damage not only from a health system perspective, but also to economies and morale in Uganda and beyond.
Governments will not be able to provide all the solutions. Seed Global Health and other organisations have teams on the ground ready to support but we need to unlock and mobilise flexible support to help create the response required to meet the threat of a broader outbreak.
In the long term, this latest outbreak underlines the critical need to invest in health system resilience — built on the strong foundations of much greater investment in the health workforce — one that is able to meet the entire spectrum of diseases we face. Over the last decade we have helped to train over 5,000 health workers in Uganda alone.
Front-line health workers in Uganda are not only protecting the Ebola patients in their care but the entire world. Urgently creating surge capacity, building resilience to protect health care workers from burnout, providing equipment and training to keep them safe while identifying, managing, and isolating Ebola patients is the best strategy to contain the outbreak. This should not only be a knee-jerk response in the face of an outbreak but the status quo going forward.
One of the biggest lessons of the COVID-19 pandemic has been that no one is safe until everyone is safe. We cannot afford to make the same delayed response again. We must support immediate action on the ground in Uganda now.
After all, if we fall now, at the first hurdle, what hope does that provide for the next pandemic?
****
Irene Atuhairwe Duhaga is the Uganda country director at Seed Global Health, leading and providing oversight in strengthening health systems in the country through education, practice and policy. Dr. Vanessa Kerry contributed to this article. She is CEO at Seed Global Health and directs the global public policy and social change program at Harvard Medical School.
Source:DEVEX
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price