
Health Minister Aceng’s recipe for success or failure?
Kampala, Uganda | THE INDEPENDENT | Uganda has the ability to effectively respond to its first Ebola virus outbreak in more than a decade and to curb its spread to other regions and neighbouring countries.
That is the expressed view of the World Health Organisation (WHO), Uganda’s health ministry, and the Africa Centres for Disease Control (CDC).
“Uganda is no stranger to effective Ebola control. Thanks to its expertise, action has been taken quickly to detect the virus and we can bank on this knowledge to halt the spread of infections,” said Matshidiso Moeti, WHO Regional Director for Africa.
The experts have also noted that Uganda is battling the Ebola Sudan virus whose outbreaks tend to be small, making chances of successful control higher for the outbreak that was officially declared on Sept. 20.
But there are dark clouds hovering above the optimism. There is no vaccine for the Sudan strain of Ebola virus and Uganda’s strategy is to prevent infections and manage through early supportive care.
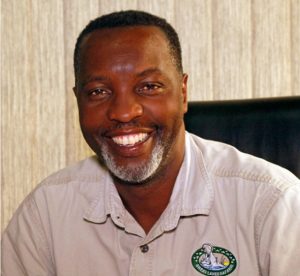
The strategy has been under strain over what appears to be a turf fight between the Ministry of Health, led by Dr. Jane Ruth Aceng – a respected figure in the fight against viruses in Uganda and beyond, and the Uganda Virus Research Institute (UVRI) led by Prof. Ponsiano Kaleebu – an equally distinguished virologist. This has led to speculation that the public is not getting all the information that it should be getting about the outbreak.
Many people commenting on how Dr. Aceng is running the response to the Ebola outbreak have pointed at the pressure she must be under. Barely rested from battling the Covid-19 pandemic over a two-year period, she is back in the trenches. She is applauded for the successes and blamed for the failures. What will it be when Ebola ends?
Experts on how to respond to an Ebola outbreak such as Dr. Mosoka Fallah; one of those who managed the 2014/2015 Ebola outbreak in West Africa, say getting the right information is very important to succeeding.
“Misinformation, disinformation and rumours make response efforts difficult. It can create great hostility to response teams,” he wrote recently in an essay published by the online journal, The Conversation.
Communicating the risk the disease poses was one of the success factors highlighted in a case study by ThinkWell sponsored by the Bill & Melinda Gates Foundation. Titled “Uganda’s Emergency Response to the COVID-19 Pandemic: A Case Study.” It was published in September 2020.
It points at how Uganda’s Ministry of Health stressed the importance of communication for COVID-19 and shared information via presidential speeches, television and radio broadcasts, posters, social media, and COVID-19 communication resources online where latest information was uploaded. Some of these interventions have been missing in the ongoing Ebola response.

Don’t panic
Mostly, there has been emphasis of spreading feel good information. This is the strategy that Great Lakes Safaris and Uganda Lodges CEO, Amos Wekesa, has been pushing.
On Oct.03 he tweeted: “While at a new hotel Nakasero last Thursday, one of the heads says immediately Ministry of Health made Ebola announcement, 167 rooms booked were cancelled. The guests were coming for a conference for a whole week and my mind run to the onion, tomato supplier, transporters etc.!
“They have same hotels in Tanzania and Rwanda and he says their branch in Rwanda is doing 85% occupancy throughout the year because of the conferencing business! He says it’s how the message was put out, no regard for business.”
Amos Wekesa was in 2015 appointed to the global ‘Africa is not Ebola’ campaign set up to spread feel good information about the continent following the West African outbreak. They argued that although Ebola has struck the continent, tourists, investors and consumers should not be scared to visit because the situation is not as grim as presented. They say such reporting hurts the economy.
Possibly as result, by Oct. 20, the Ministry of Health was reporting that there were 64 confirmed Ebola cases in the country and 25 confirmed Ebola deaths.
But a day earlier, on Oct.19, the World Health Organisation (WHO) had announced that there have been 60 confirmed and 20 probable cases since the outbreak began in September, and 44 deaths. The differing numbers are confusing to the public and are a result of the Ministry of Health’s refusal to include in the official death numbers people who likely died of Ebola before the outbreak was confirmed.
The WHO said eight most recent Ebola cases reported on Oct.20 have no known links with known patients, raising concerns over the spread of the deadly disease. It said initial investigations into the cases by the Ministry of Health had shown they were not contacts of people already known to have Ebola.
“We remain concerned that there may be more chains of transmission and more contacts than we know about in the affected communities,” WHO Director General Tedros Adhanom Ghebreyesus told reporters.
The Ministry of Health did not release this information to the public.
In another incident, President Yoweri Museveni on Oct.15 revealed that an Ebola infected person had travelled by taxi from Mubende to Kibuku in eastern Uganda to attend a burial.
“I don’t know why these people have not released that information,” he said, meaning the officials of the Ministry of Health.
The President who was addressing the nation to give an update on Ebola, announced a 21-day lockdown on districts of Mubende and Kasanda. He said it was failure of locals to adhere to directives and advice by the Ministry of Health had prompted the lockdown.
“This was very easy to stop if the people of the other village had listened. I told people stay home but you hear one went to Luweero and then to Kampala. He died. Another one has gone to Kibuku,” he said.
The lockdown came as a surprise because just two weeks earlier, President Museveni and Dr. Aceng had announced that lockdowns over Ebola were unwarranted as the disease was easy to control.
“The problem comes if I touch where a sick person smeared me with something and then I touch soft parts of the body parts like eyes, nose and mouth. That is when the virus will enter your body. Therefore, when we heard about these characteristics of Ebola, we decided to fight differently. It is not necessary to have lockdowns, to close schools, stop you from going to churches, markets or travelling,” Museveni said.
He added: “I want to reassure Ugandans and all residents that the government has the capacity to control this outbreak as we have done before. Therefore, there’s no need for anxiety, panic, restriction of movement or unnecessary closure of public places like schools, markets, places of worship etc. as of now,” he said.
Missing information
The lockdown announcement made it appear that the government did not have the Ebola situation under its control and was fire-fighting.
The announcement of an Ebola case in the capital Kampala also created the impression of a Ministry of Health determined to ensure that the Ebola outbreak is battled “quietly.”
Minister Aceng confirmed that an Ebola patient who had self-reported and been admitted to Kiruddu National Referral Hospital in Kampala had died on Oct.07. At time of death, the patient was not being treated for Ebola but his Ebola infection was confirmed posthumously from a sample that had been taken from him before he was buried.
Minister Aceng confirmed this. But she was also very firm on the case being referred to as a Mubende case and not a case in Kampala.
“I want to state very clearly that this does not mean Kampala has Ebola,” Aceng told reporters,” Cases that were already listed in Mubende remain cases of Mubende. Unless Kampala generates its own cases that start within Kampala, we cannot call that a Kampala case.”
Local media outlets followed Dr. Aceng’s lead on the “quiet” Ebola and did not push the issue. But foreign media refused to allow Aceng’s constraints.
“Uganda says Ebola has not reached capital, despite cases,” announced the Medical Express publication, which is part of the Science X network; one of the largest online communities for science-minded reaching 10 million readers. Other major media outlets such as the BBC, the New York Times, Reuters and more reported the story in a similar way.
Days later, it emerged that another person had caught Ebola in the capital Kampala. Minister Aceng confirmed the case and said the woman who had just given birth was the wife of the man who had died of Ebola earlier in Kiruddu Hospital.
Before Aceng’s announcement, the woman was attended to by several medical personnel as she delivered a baby. The status of the health officials who were treated at Mulago National Referral Hospital and the new baby born, remain unclear.

Fight over strategy
Much earlier, on Oct.06 at a meeting of the Ebola Task Force in Mubende District which is the epicenter of the current Ebola outbreak, Aceng announced that UVRI staff are not allowed to operate in the Mubende Ebola Treatment Unit (ETU).
“I now state it clearly that if you are the UVRI staff and still here, please go,” she said, “No research will be conducted without my knowledge, never! And it has ended.”
The UVRI works under the Ministry of Health but is semi-autonomous; with its own budget vote. The UVRI is mandated to conduct epidemiological research and data management and support response to disease outbreaks. It is also mandated to carry out virological research to generate new knowledge and to lead to disease prevention and intervention strategies in Uganda and internationally.
Tackling major disease outbreaks usually commands big budgets and it’s not uncommon for officials to disagree over control. According to a study in the `Journal of Infectious Diseases’ an Ebola outbreak that ravaged Sierra Leone, Guinea and Liberia in 2014 cost economies an estimated US$53 billion.
The 2003 severe acute respiratory syndrome (SARS) cost an estimated US$40 billion, while the 2015-2016 Zika virus outbreaks in the Americas was estimated to have caused $20 billion in social costs, the study said.
In an article titled `Uganda’s Covid-19 Supplementary Budget: Pandemic Response or Cash Bonanza?’ published in the journal of the social science research institute, CMI of Norway, Prosscovia Nambatya, an Advocate of the High Court of Uganda who keeps a keen eye on public finance and expenditure in Uganda, described how government departments tussled to get COVID-19 money.
“Although the Ministry of Health is the lead agency in the fight against Covid-19, other ministries and agencies have allocated themselves similar responsibilities in order to get a share of the Covid-19 supplementary budget. This paints a bad picture of a scramble for and partition of public resources,” she wrote.
Similar tussles led to the ouster of former Uganda Aids Commission (UAC) board chairman, Prof Vinand Nantulya by then UAC boss, Dr. Christine Ondoa in 2016. Ondoa was Minister of Health from 2011 to 2013.
Nantulya was accused of having an autocratic management style and the two reportedly fought over religious beliefs colouring their work. Prof. Nantulya, a distinguished researcher and medical entrepreneur was also pushed out as chairman of the Ugandan Health Policy Panel, the Uganda Country Coordinating Mechanism (UCCM) overseeing programmes funded by the Global Fund.
In another case, Prof Anthony Mbonye, one of the county’s most published medical authors, was pushed out as Director-General of health services in 2017. He wrote a damning book on infighting in the Health ministry titled `Uganda’s Health Sector Through Turbulent Politics, 1958-2008’. Dr Aceng has been Minister of Health since 2016.
Prof. Pontiano Kaleebu, the UVRI Director, when asked by the Daily Monitor about the orders from the minister, reportedly said: “I don’t want to talk about that issue.”
However, Prof Kaleebu also said they have been doing research on suspected Ebola patients and that through this, recently, they were able to detect the second case of Crimean-Congo haemorrhagic fever (CCHF). Still, in the Mubende meeting, Dr Aceng banned the double sample collection from Ebola suspects.
“It has come to my notice that two blood samples are still taken from a single patient at the ETU. This must stop. The government will not entertain a second party trying to manipulate and interfere by way of research through unauthorized means. It is one blood sample per person,” Dr. Aceng said.
The UVRI is Uganda’s top virus research body and has in the past been at the centre of testing of samples of suspected viral diseases like Ebola, HIV, Marburg, Zika, SARS and COVID-19.
When the Ministry of Health announced the first confirmed case in the outbreak of Ebola in Mubende, it referred to tests done at UVRI.
The Ministry said the case was a 24 year old male from Ngabano Village in Madudu Sub-County, who was referred to and admitted and isolated at Mubende Regional Referral Hospital.
He had high-grade fever, tonic convulsions, blood-stained vomit and diarrhoea, loss of appetite and pain while swallowing starting on Sept.11.
“A blood sample was collected and analysed at the Uganda Viral Research Institute (UVRI) laboratory on 18 September 2022. The result was reported on the 19th with a confirmed positive result for EVD (Sudan strain),” the Ministry said. After five days of hospitalization, the patient died on 19 September 2022.
Despite this early collaboration, it has emerged that the Minister of Health, Dr. Aceng, has blocked UVRI from involvement in activities around the fight against the Ebola virus.
Instead, according to the Daily Monitor newspaper citing highly placed sources in the government, the minister has given the powers of testing of Ebola to Kampala-based Central Public Health Laboratories (CPHL), which is directly under the Health ministry.
The vaccines used successfully to curb recent Ebola outbreaks in the Democratic Republic of the Congo are not effective against the type of Ebola virus that is responsible for this outbreak in Uganda. However, several vaccines are in various stages of development against this virus, two of which could begin clinical trials in Uganda in the coming weeks, pending regulatory and ethics approvals from the Ugandan government.
The tension is between scientists interested in carrying out research and those determined to care for the patients. Some caregivers may feel that providing clinical care and conducting clinical research cannot be combined and one could not be done without harming the other effort. But best practice seeks to integrate research into clinical care.
Clinical care focuses on the individual, current needs of a specific patient, while clinical research benefits future patients and not necessarily the specific patient enrolled in the research.
“The urgent desire to help current patients with whatever is available may appear to be in conflict with the need to learn as much as possible about potential interventions in order to help current and future patients,” said a report titled ‘Integrating Clinical Research into Epidemic Response: The Ebola Experience’ by the National Academies of Sciences, Engineering, and Medicine.
It said, in 2014, as the Ebola epidemic rapidly spiraling out of control in West Africa, some experts suggested using experimental medicinal products to treat Ebola patients.
The WHO and some NGOs treating the patients refused. They feared that using untested medical products could fuel already existent mistrust, conspiracies, and even violence toward health workers. There were rumours that the international scientists were spreading disease, harvesting organs, and other horrible things.
Uganda has previously successfully battled Ebola outbreaks and snuffed them out in no time. But an Ebola outbreak has potential to run out of control with devastating consequences.
The West African outbreak in Sierra Leone, Guinea and Liberia ran for four years, from 2013 to 2016 and killed at least 11,300 people, and cost the economies an estimated $53 billion. To date, those countries have not recovered. That is what Dr. Aceng is trying to avoid.
****
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price


The culture of observing appropriate Biosafety practice and ensuring sustained activity seems to be getting lost in this country
There is a price to pay
Let those who see this problem be on the alert